By Aman Kabra, Analyst, MIHM
Hypertension is the number one health-related risk factor in India, with the largest contribution to the burden of disease and mortality.[i] It has been the single most significant cause of death in India for the last 15 years[ii], accounting for 0.8 million deaths out of the 9.6 million recorded deaths in 2016. Hypertension is exerting an increasingly substantial public health burden on India’s healthcare system; disability-adjusted life years (DALYs) attributable to hypertension increased from 21 million in 1990 to 39 million in 2016 (+89%)[iii]. Furthermore, more than half of the hypertensive population in India is not even aware of their high blood pressure condition.[iv] Among those diagnosed with hypertension, only one-tenth of rural and one-fifth of urban Indians have their blood pressure (BP) under control.[v]
Secondary data reveals that 42% of all Indians who suffer from hypertension reside in small towns[vi]. They visit indigenous private practitioners who do not regularly screen for hypertension due to limited resources. Formal healthcare in such small towns is not sought by the patients until seriously ill. Small towns in India are currently in the transitional phase. Despite a ten times increase in hypertension prevalence in small towns of India in the past six decades[vii], there is a scarcity of studies that attempt to understand hypertension management in such geographies. Moreover, private practitioners[1] are the first point of contact for curative healthcare for the majority of such populations[viii],[ix]. It is, therefore, imperative to understand the role of private practitioners in the awareness, diagnosis, and treatment of hypertension in small towns. William C. Hsiao, in his research, highlights the collision between incentives and professionalism for private providers[x]. Incentives often shape private providers’ professional behaviours; these incentives could be formal and monetary, such as pharmaceutical incentives, as well as unorganized and informal such as word-of-mouth feedback in the community. Effective interventions targeted at private providers in small towns are a necessity to achieve WHO’s targets of a 25% reduction in premature non-communicable disease (NCD)-related mortality by making significant inroads in hypertension care in India. An exploration of the roles of private practitioners in hypertension management is a necessity for designing such interventions.
The ISB team conducted a field visit to interview private practitioners in the small town of Karimnagar, Telangana. The qualitative study aimed at understanding the practitioners’ practices for hypertension management, their adherence to the prescribed guidelines, dynamics of referral chain throughout the patient care pathway, and the practitioners’ motivation to alleviate hypertension through collaborative programmes. Hypertension prevalence in Telangana is similar to its average prevalence in India [13% and 20% compared to India’s average of 11% and 15% among women (15-49y) and men (15-54y), respectively][xi]. Also, diabetes, a common co-morbidity with hypertension and a significant risk factor for cardiovascular disease events, has a very similar prevalence in Telangana compared to the national average. The insights from this study, therefore, help understand hypertension management across various geographies with demographic profiles similar to Telangana, such as Andhra Pradesh, Chhattisgarh, and Tamil Nadu.
The majority of the certified practitioners[2] at Karimnagar consider systolic BP of > 160 mm and/or 110 mm diastolic as the BP threshold for diagnosing hypertension, whereas the standard threshold for the diagnosis of hypertension, as laid down by the Ministry of Health & Family Welfare, Government of India, is persistent elevation of systolic BP of > 140 mm and/or 90 mm diastolic. As mentioned by a Karimnagar super-specialist, the practitioners’ reservations to prescribe hypertension medication to early-stage hypertensive patients stems from their reluctance towards spending additional face-time with these patients (hypertensive patients need to be counselled by the practitioners about lifestyle modifications and suitable dietary habits, in addition to being prescribed hypertensive medication).
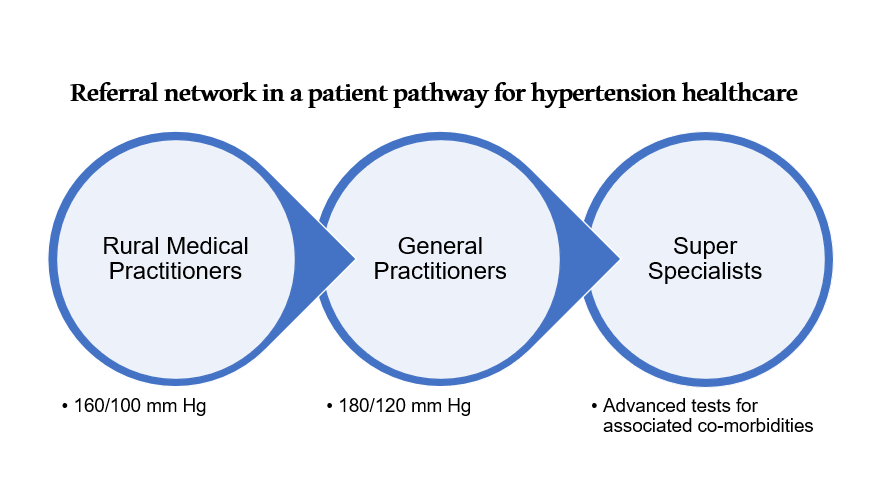
We also sought information on referral patterns among provider networks. The players [rural medical practitioners (RMPs), general practitioners (GPs), super-specialists, pharmacies, and diagnostic laboratories] across various segments of the care-pathway have established symbiotic alliances for referral gains. Small towns are typically remotely located and a large number of RMPs are present in these towns. Therefore, the majority of rural patients visit RMPs as the first contact point for consultation. RMPs refer high-grade hypertensive patients to a GP in their network, who, in turn, refer patients to a super-specialist in case of hypertensive crisis (systolic BP of > 180 mm and/or 120 mm diastolic).
GPs in Karimnagar typically charged INR 250 for the first consultation visit and INR 200 for the follow-up visits. RMPs receive a commission of 30% to 50% of the first-consultation fee from the GPs for each referral of a hypertensive patient. Several instances of private practitioners’ over-prescribing of diagnostic tests have been noted at Karimnagar. This is directly attributed to referral incentives from diagnostic laboratories to the prescribing practitioners. The diagnostic laboratories incentivize the referring practitioners with 25-30% of the fee received from each diagnostic test. GPs and super-specialists do not usually engage with pharmacists for referral gains. These practitioners, however, tend to stock commonly prescribed hypertensive medication at their clinics; they monetize the discounts received from pharmaceutical companies for promoting their medicine brand by selling the medicines at the maximum retail price.
Certified practitioners in Karimnagar have observed that certain RMPs suggest patients refrain from allopathic hypertension treatment unless BP reaches a worrisome figure, typically above 160/110 mm Hg. Since RMPs are the first point of contact for the majority of the rural patients, they are quite influential in steering the patients towards a specific treatment course. Other unprincipled practices of RMPs that have been brought to light include home-delivery of medicines to retain patients and prescribing symptomatic treatment instead of the root-cause addressal of hypertension.
We also noted that Karimnagar pharmacies frequently dispense medicines without demanding a medical prescription. The majority of long-term hypertensive patients prefer a direct consultation and medicine purchase at a pharmacy to paying a follow-up consultation fee to the certified practitioners. Such practices are un-regulated, lack credible medical knowledge, and are merely intuition driven.
Furthermore, Karimnagar commoners lack awareness about the adverse effects of uncontrolled hypertension, perhaps primarily due to the reluctance of practitioners to spend educational face-time with hypertensive patients. One of the GPs, currently in his mid-50s, commented, “Though the majority of these hypertensive patients are in their forties (age), I’m deeply concerned about the young folks being increasingly diagnosed with hypertension and the co-morbid conditions. Thanks to their sedentary lifestyle!” To exacerbate the situation, hypertensive patients in Karimnagar prefer episodic care to hypertensive symptoms, such as headache, tingling sensations, and heavy perspiration. There also exists a social stigma among patients about labelling themselves as ‘hypertensive’ or ‘diabetic’. This stigma contributes to the patients’ early drop-out from the prescribed long-term hypertension treatment. A super-specialist at Karimnagar adds, “I have noted several instances of provider hopping and sub-optimal follow-ups by hypertensive patients, which reflects in poor drug adherence among these patients.”
There are several issues in hypertension management at the private healthcare supply end, which need to be understood before effective interventions can be designed. Achieving a sustainable model for long-term hypertension management needs to be the broader objective instead of improving episodic care. Small towns continue to have a fragmented provider base. The real challenge in improving hypertension management is to devise a healthcare solution that is not only cost-effective but also scalable to multiple geographic locations for a sizeable impact on hypertension healthcare of the country as a whole.
References
[1] Private practitioners refer to the healthcare providers who work independently as healthcare practitioners and are not employed by Central or the State Government. They include (i) Modern medicine providers i.e. certified allopathic doctors who are recognized by the medical board and are licensed to practice medicine, (ii) AYUSH (Ayurveda, Yoga, Unani, Siddha and Homeopathy) practitioners i.e. non-allopathic doctors who are licensed to practice biomedicines by the regulatory authority, (iii) Informal care providers i.e. practitioners such as quacks, pharmacist, healthcare workers who are not trained formally by a recognized institution but provide informal care.
[2] Certified practitioners are healthcare providers who are authorized to practice as defined by governing laws of the country. They include (i) Modern medicine providers i.e. certified allopathic doctors who are recognized by the medical board and are licensed to practice medicine, and (ii) AYUSH (Ayurveda, Yoga, Unani, Siddha and Homeopathy) practitioners i.e. non-allopathic doctors who are licensed to practice biomedicines by the regulatory authority
[i]Ministry of Health & Family Welfare, G. o. (2016). Hypertension: Screening, Diagnosis, Assessment, and Management of Primary Hypertension in Adults in India. India: Ministry of Health & Family Welfare.
[ii] Global Action Plan for Prevention and Control of Non-communicable diseases 2013-20. World Health Organization. Accessed at http://apps.who.int/iris/bitstream/handle/10665/94384/9789241506236_eng.pdf?sequence=1 on January 19, 2019.
[iii] Gupta, R., Gaur, K., & Ram, C. V. S. (2019). Emerging trends in hypertension epidemiology in India. Journal of human hypertension, 33(8), 575-587.
[iv] https://qz.com/india/1612482/why-hypertension-high-blood-pressure-can-be-fatal-in-india/
[v] Anchala, R., Kannuri, N. K., Pant, H., Khan, H., Franco, O. H., Di Angelantonio, E., & Prabhakaran, D. (2014). Hypertension in India: a systematic review and meta-analysis of prevalence, awareness, and control of hypertension. Journal of hypertension, 32(6), 1170.
[vi] Anchala, R., Kannuri, N. K., Pant, H., Khan, H., Franco, O. H., Di Angelantonio, E., & Prabhakaran, D. (2014). Hypertension in India: a systematic review and meta-analysis of prevalence, awareness, and control of hypertension. Journal of hypertension, 32(6), 1170.
[vii] Kokiwar, P. R., Gupta, S. S., & Durge, P. M. (2012). Prevalence of hypertension in a rural community of central India. J Assoc Physicians India, 60(6), 26-9.
[viii] Gautham, M., Binnendijk, E., Koren, R. and Dror, D.M., 2011. ‘First, we go to the small doctor’: The first contact for curative health care sought by rural communities in Andhra Pradesh & Orissa, India. The Indian journal of medical research, 134(5), p.627.
[ix] De Costa, A. and Diwan, V., 2007. ‘Where is the public health sector?’: Public and private sector healthcare provision in Madhya Pradesh, India. Health Policy, 84(2-3), pp.269-276.
[x] Hsiao, W. C. (2008). When incentives and professionalism collide. Health Affairs, 27(4), 949-951.
[xi] International Institute for Population Sciences (IIPS) and ICF. 2017. National Family Health Survey (NFHS-4), 2015-16: India. Mumbai: IIPS.

